FRANKFORT — The Interim Joint Committee on Health Services received updates from major health care groups Wednesday about COVID-19’s impact and workforce shortages in Kentucky.
Those representing the state’s Cabinet for Health and Family Services, the Kentucky Association of Health Care Facilities and Kentucky Center for Assisted Living, the Kentucky Nurses Association, and the Kentucky Medical Association testified. Legislators had a full gamut of questions following their presentations.
Committee members heard about a shortage of physicians and nurses in the state and how health groups plan to move forward regarding COVID-19.
Patrick T. Padgett, executive vice president for the Kentucky Medical Association, told legislators that between 2019 and 2022, Kentucky’s physician count fell from 10,592 to 10,002. This statistic is credited to the Kentucky Office of Rural Health’s 2022 Kentucky Physician Report.
“We lost 590 physicians out of the state at a time that we needed more physicians in the state. So that’s a big loss, and physicians not only treat patients and try to maintain their health and make them healthier and make them more productive, but they are an economic driver in the state,” he said.
According to a recent study of the American Medical Association, on average, physicians each bring about $1.9 million of economic activity to a region, Padgett said.
“So when we lost 590 physicians, Kentucky lost over $1 billion in economic impact,” he said.
Sen. Karen Berg, D-Louisville, is a physician who serves on the committee. She said prior authorization from insurance companies can be “out of control” because of administrative burdens. She also raised concerns that far too many medical students say they’re planning to leave Kentucky.
“These first- and second-year medical students, and I would say there’s at least 40 in the room when I’m talking, are telling me that under no circumstances are they planning on doing their residencies here in Kentucky. They are all planning on going away,” she said.
As is the case with physicians, the nursing field is experiencing shortfalls, testified Delanor Manson, chief executive officer of the Kentucky Nurses Association.
“Pre-pandemic, there was a nursing shortage. The pandemic did not cause the nursing shortage. On average, the Kentucky nurse is 53 years old. Nurses in the rest of the country are 42,” she said. “Things such as inflexible work schedules, unsafe work places, nurses being absent from decision-making in organizations, nurse retention and the image of nursing have played a part in the nursing shortage.”
In a separate presentation, officials from the Cabinet for Health and Family Services reported that COVID-19 statistics have changed over time, and the information will be studied for decades.
CHFS Secretary Eric Friedlander offered a brief critique of how the pandemic has been handled, and said it’s now moving to an endemic stage.
“There were good decisions made. There were bad decisions made, and we’re going to parse that out as folks examine what was effective, what wasn’t, what had an impact, what didn’t,” he said. “I promise you we were going with the best of our knowledge, and it changed over time.”
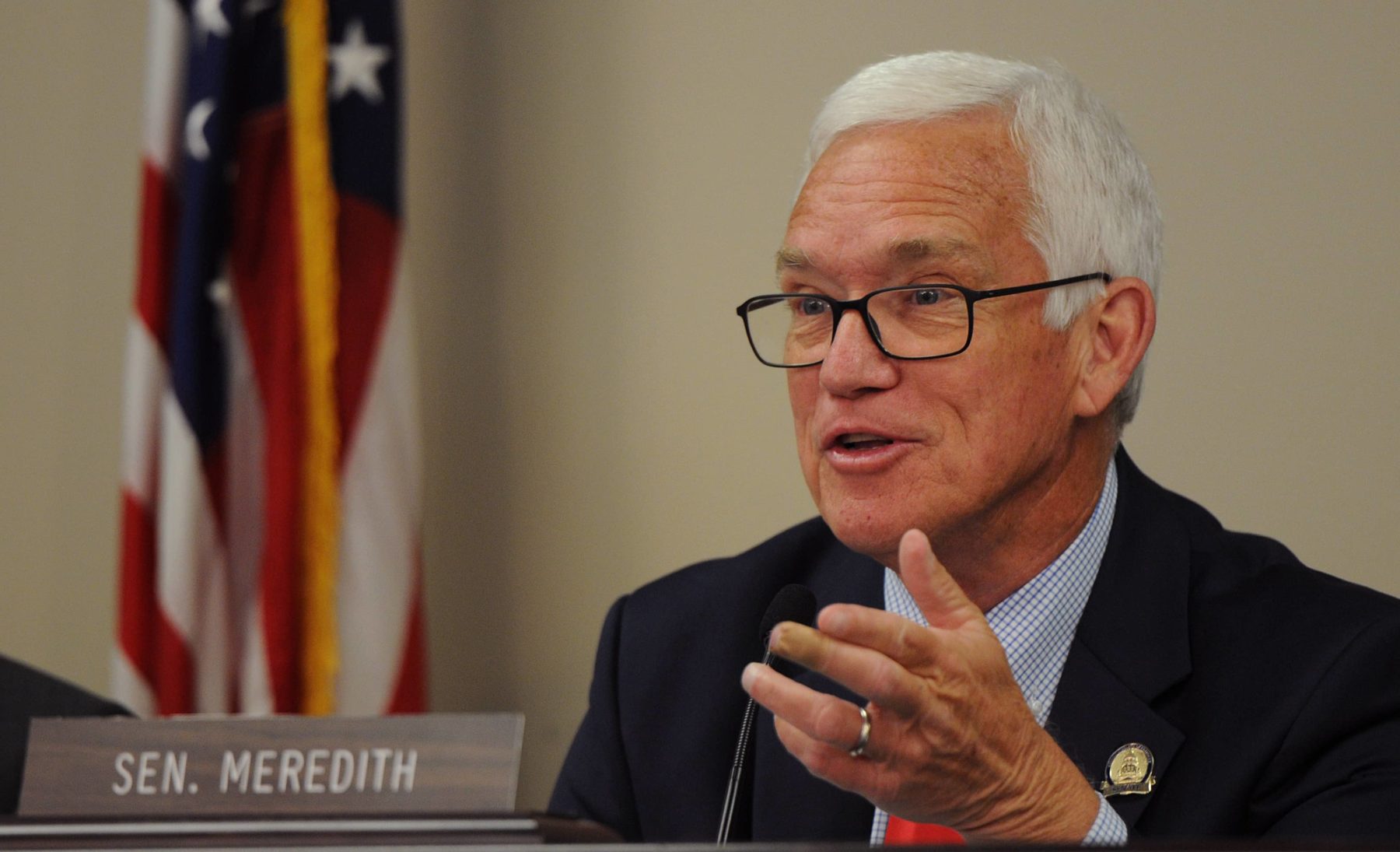
Sen. Stephen Meredith, R-Leitchfield, co-chair of the committee, asked Friedlander about the number of Medicaid recipients in Kentucky. He said he’s concerned about the program’s future cost.
“Let me put some historical perspective on this. In 2017, we had, I think, 1.4 million Medicaid recipients. The Medicaid budget was $10 billion. Going forward to this year, we’re at 1.7 million, $15 billion budget,” he said. “A lot of tremendous economic push and pull on this that I’m not sure we’ve factored in. We haven’t talked about the impact of inflation at all on this program.”
Sen. Shelley Funke Frommeyer, R-Alexandria, asked how people could be encouraged to transition to private plans so taxpayers aren’t covering their insurance.
“Is there something that we legislators can do to promote that gradual move off of Medicaid…” she said.
Friedlander said it’s an economic development question and getting people “living wage” jobs.
Veronica Judy-Cecil, deputy commissioner of CHFS’s Department for Medicaid Services, added that every Medicaid recipient has the opportunity to complete job training and they are connected to the Kentucky Education and Labor Cabinet.